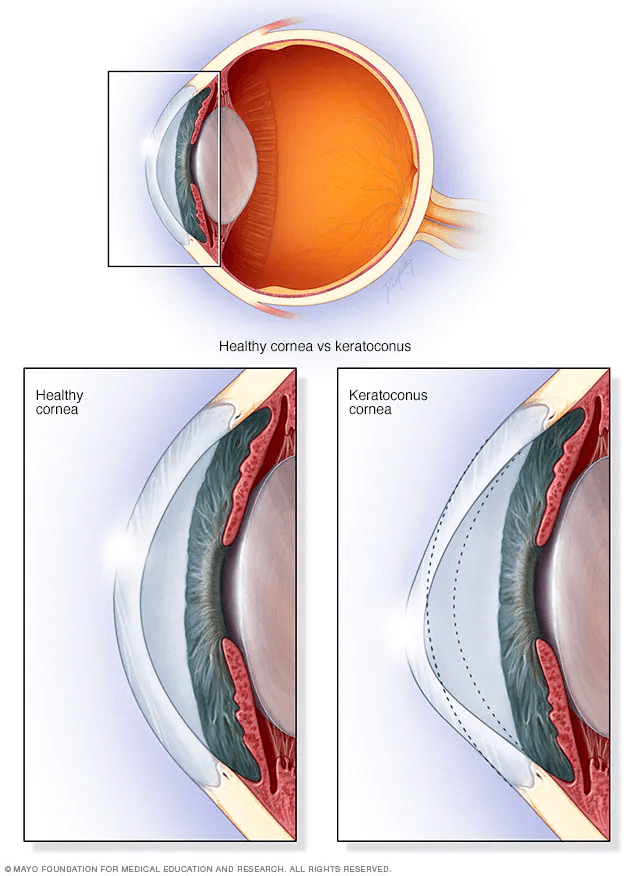
Keratoconus is an eye condition that causes the cornea to become progressively thinner. A normal cornea is round or spherical in shape, but with keratoconus the cornea bulges forward, assuming more of a cone shape. As light enters the cone shaped cornea it is bent and distorted and unable to come to a point of clear focus on the light-sensitive retina.
Keratoconus usually affects both eyes but the two eyes often progress at different rates. This disease typically begins during teenage years. In most patients, it progresses for several years before stabilizing in the third to fourth decade of life. In severe cases it can continue to worsen. In these cases the cornea continues to thin and bulge outward, further blurring vision. Scarring of the cornea can also develop.
Clinical studies have shown Acupuncture is effective in a wide range of disorders including Eye Diseases, Diabetes, Hyperthyroidism, Hypothyroidism, Hashimoto, Cushing’s Syndrome, Osteoporosis, Thyroiditis, PCOS / Addison’s Disease and Menopause.

Increases Ocular Circulation.

Reduces Inflammation and Increases Circulation.

Non-Surgical and Opioid-Free treatment.

No side effects and safe.

Releases Endorphins to combat pain.


Ayurveda offers one of the most effective medicines for digestive issues and helps to correct root cause of your condition.

Complete holistic healing system in existence more than 3000 years.

Based on the concept of root-cause diagnosis and management.

Focuses equally on prevention and cure to improve quality of life.

Helps identify and recommends foods for your body type and condition.
Herbal medicine has a history of at least several thousand years and uses mostly plants to treat diseases and promote health.
Can successfully treat many chronic and complex conditions.

Clinically and scientifically proven to treat a wide range of complex eye conditions.

Safe and has relatively less side effects.

Helps boost your immune system naturally.

Shown to reduce stress and relieve anxiety.

Improves respiratory and cardiovascular function.


Therapeutic Yoga or Yoga Therapy involves employing a variety of yoga practices to help improve a health.It also adapts the practice of Yoga to the needs of people with specific health condition.

Improves strength, balance and flexibility.

Helps with chronic pain relief.

Improves circulation and reduces blood pressure.

Reduces stress and improves sleep.

Improves respiratory and cardiovascular function.
Researchers believe that approximately 3 million people worldwide have keratoconus. It affects males and females of all races throughout the world. The causes are still being researched, but the likelihood of developing keratoconus is greater if you:
The below factors can also contribute to your Glaucoma progression.
Neuroprotection therapy helps protect neurons in your eye from injury such as from eye pressure elevations. Neurotrophins helps to provide the required neuroprotective therapy which prevents from death of the ganglion cells in your eyes.
Vascular dysregulation means that blood flow is not properly flowing. This causes reduced and unstable oxygen supply to the tissues in the eyes. This in turn causes a cacade of events causing glaucomatous optic neuropathy.
Oxidative stress damage is an important factor in development of glaucoma, which triggers trabecular meshwork degeneration, which then leads to intraocular hypertension. Different studies provide cumulating evidence, which supports the association of oxidative stress with different aspects of the neurodegenerative process happening in glaucoma.
Glaucoma is associated with toxic inflammatory factors leading to cell death and disease progression. Trabecular meshwork dysfunction is likely mediated by oxidative stress and inflammatory responses. Ocular surface inflammation may compromise the cornea, conjunctiva and the trabecular meshwork.
Excitotoxicity is increased levels of glutamate and is seen in Glaucoma patients which cause
retinal ganglion cell (RGC) death. If the toxic effects of glutamate aren't blocked, RGC loss can continue, leading to further visual impairment.
Netra Restoration Therapy provides the following benefits for patients with Glaucoma.
The level of loss of nerve fiber layer and optic nerve atrophy will determine the level of the improvement seen.
Most patients start to see subjective improvements in their vision within just 7 days of starting the NRT treatment.
NRT treatment can stop Glaucoma vision loss progression or considerably reduced to preserve the remaining vision.
NRT treatment improves visual field by reinstating dormant and sub-optimally functioning retinal cells. Without treatment these cells would eventually neurodegenerate and be lost forever.
With NRT treatment most glaucoma patients have shown improvement in their visual acuity by a minimum of 1 to 2 lines in distant and near vision.
Most glaucoma patients treated with NRT treatment have shown marked improvement in their color contrast.
Most glaucoma patients treated with NRT treatment have experienced having brighter vision, a reduction in glare, and blurry/cloudy vision.